Increasing Liver Stiffness is Associated with Adverse Outcomes in Individuals with Fontan Circulation
Samuel W. Brayer, MD; Tarek Alsaied, MD; Joseph J. Palermo, MD; Alexander R. Opotowsky, MD; Nicole Brown, MD; Hassan Almeneisi, MD; Andrew T. Trout, MD; Jonathan R. Dillman, MD, MSc, Adam M. Lubert, MD
As children with congenital heart disease age into adolescence and adulthood, it’s important to develop non-invasive and reliable biomarkers for progression of extra cardiac disease; serial measurement of liver stiffness via magnetic resonance elastography shows promise as a marker for clinical decompensation.
Samuel Brayer, MD
Abstract
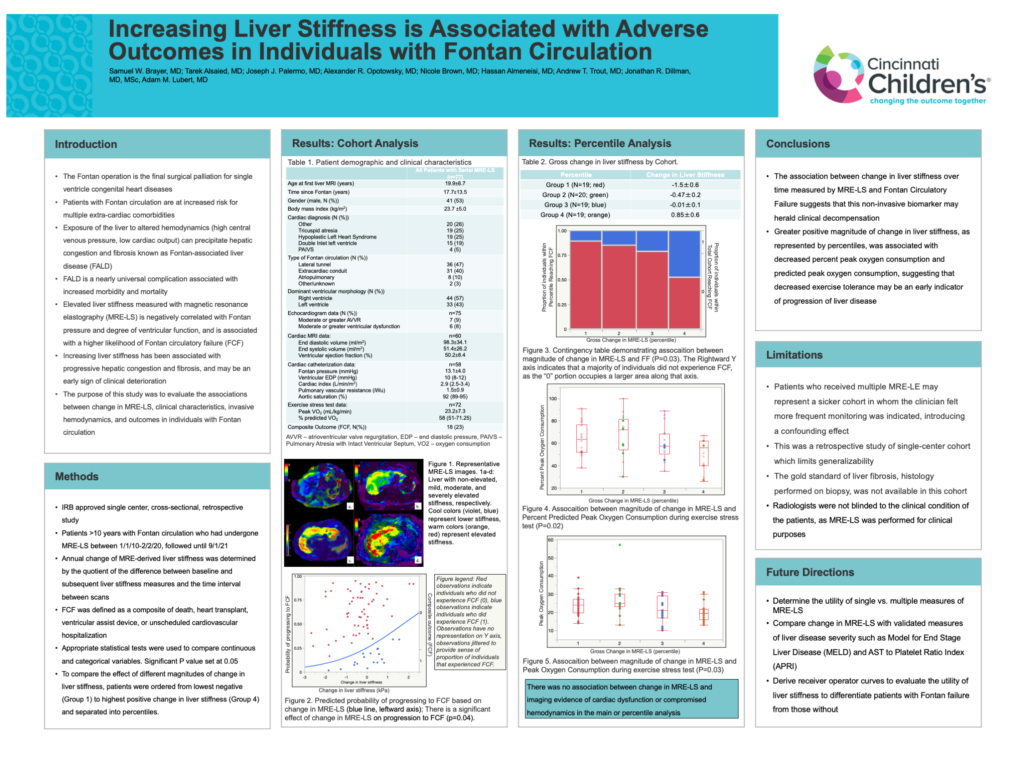
Background: Patients with Fontan physiology are at increased risk for multiple extra-cardiac comorbidities. Fontan-associated liver disease (FALD) is a nearly universal complication associated with increased morbidity and mortality. Elevated Magnetic Resonance Elastography-derived Liver Stiffness (MRE-LS) has been associated with worse clinical outcomes, compromised hemodynamics, worsening liver disease and increased morbidity and mortality. Change in liver stiffness over time has not been well studied.
Objective: To determine the effect of change in liver stiffness on hemodynamic variables and clinical outcomes.
Methods: Single center retrospective cross-sectional study of patients (aged >10 years) with Fontan circulation who underwent >1 MRE between 2010-2020. MRE-LS data were collected (kilopascals, kPa). Gross change in liver stiffness was defined as the difference between the most recent and most distant post-Fontan MRE-LS. Demographic, clinical, echocardiogram, cardiac magnetic resonance imaging, cardiac catheterization, and exercise stress test data were also collected. Fontan Failure (FF) was defined as the composite outcome of death, transplantation, ventricular assistive device, or unscheduled hospitalization. To compare the effect of different magnitudes of change in liver stiffness, patients were ordered from lowest negative (Group 1) to highest positive change in liver stiffness (Group 4) and separated into quartiles.
Results: 77 subjects met inclusion criteria (41 male (53%)). Mean age at first liver MRI was 19.9±6.7 years, with a mean time since Fontan operation of 17.7±13.5 years. Mean time between MRE-LS was 45.6±26.5 months. Mean MRE-LS at first and second MRI was 4.4±1.0 kPa and 4.1±1.1 kPa respectively, with a mean change in MRE-LS of -0.2±1.0 kPa. There was an association between change in MRE-LS and FF (p=0.04). In the subgroup analysis, there was an association between quartile and FF (p=0.03), peak oxygen consumption (p=0.03), and percent predicted peak oxygen consumption (p=0.02). There was no association between change in MRE-LS and imaging evidence of cardiac dysfunction or compromised hemodynamics in the main or subgroup analysis.
Conclusions: These data suggest that an association exists between magnitude in change in liver stiffness, clinical outcomes, and exercise tolerance. Change and MRE-LS is a potential non-invasive biomarker of clinical decompensation.