Inequitable Access: Factors Associated with Incomplete Referral to Pediatric Cardiology
Paul Warren, MD; Jeffrey Anderson, MD, MBA; Andrew Beck, MD; Huaiyu Zang, PhD; Christopher Statile MD
Patient and system level variables are associated with the rate of cardiology subspecialist referral completion. We need further research to elucidate how we can help our patients more easily complete referrals and receive subspecialty care in equitable ways.
Paul Warren, MD
Abstract
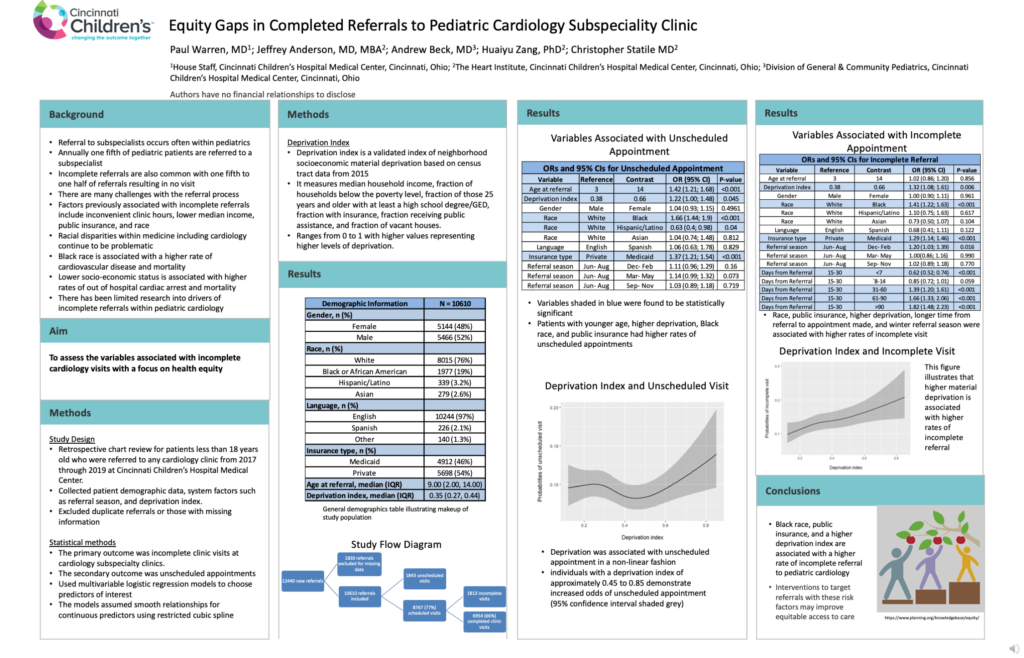
Background: Referral to subspecialists is a common and necessary occurrence in pediatrics. Socio-economic inequities may play a role in access to subspecialist care.
Objective: To assess the variables associated with unscheduled and incomplete cardiology clinic visits among referred pediatric patients with a focus on equity gaps.
Methods: We conducted a retrospective chart review for patients less than 18 years of age who were referred to cardiology clinics at a single quaternary referral center from 2017 to 2019. We collected patient demographic data, referral information, and cardiology clinic information. The primary outcome was an incomplete clinic visit. The secondary outcome was an unscheduled appointment. Independent associations were identified using multivariable logistic regression.
Results: There were 10,610 new referrals and 6,954 (66%) completed new cardiology clinic visits. Black race (OR 1.66; 95% CI 1.44-1.90), public insurance (OR 1.37; 95% CI 1.21-1.54), and a higher deprivation index score (OR 1.22; 95% CI 1.00-1.48) were associated with higher odds of unscheduled visit. Black race (OR 1.41; 95% CI 1.22-1.63), public insurance (OR 1.29; 95% CI 1.14-1.46), and a higher deprivation index (OR 1.32; 95% CI 1.08-1.61) were also associated with higher odds of incomplete visit. A shorter time elapsed from the initial referral to when the appointment was made was associated with lower odds of incomplete visit (OR 0.62; 95% CI 0.52-0.74).
Conclusion: Race, insurance type, neighborhood deprivation, and time from referral date to appointment made were each associated with incomplete referrals to pediatric cardiology. Interventions directed to understand such associations and respond accordingly could help to equitably improve referral completion.