Exploring NLRP3 Inflammasome Activity in Primary Human Macrophages in Pediatric Crohn’s Disease anti-TNF therapy Nonresponders
Molly K. Hritzo Ahye, MD, PhD; Ingrid Jurkovich, MD; Elizabeth Angerman; Lee A. Denson, MD
This project explores the role of primary human macrophages and the NLRP3 inflammasome in the response to anti-TNFalpha therapy in pediatric Crohn’s disease.
Molly Ahye, MD, PhD
Abstract
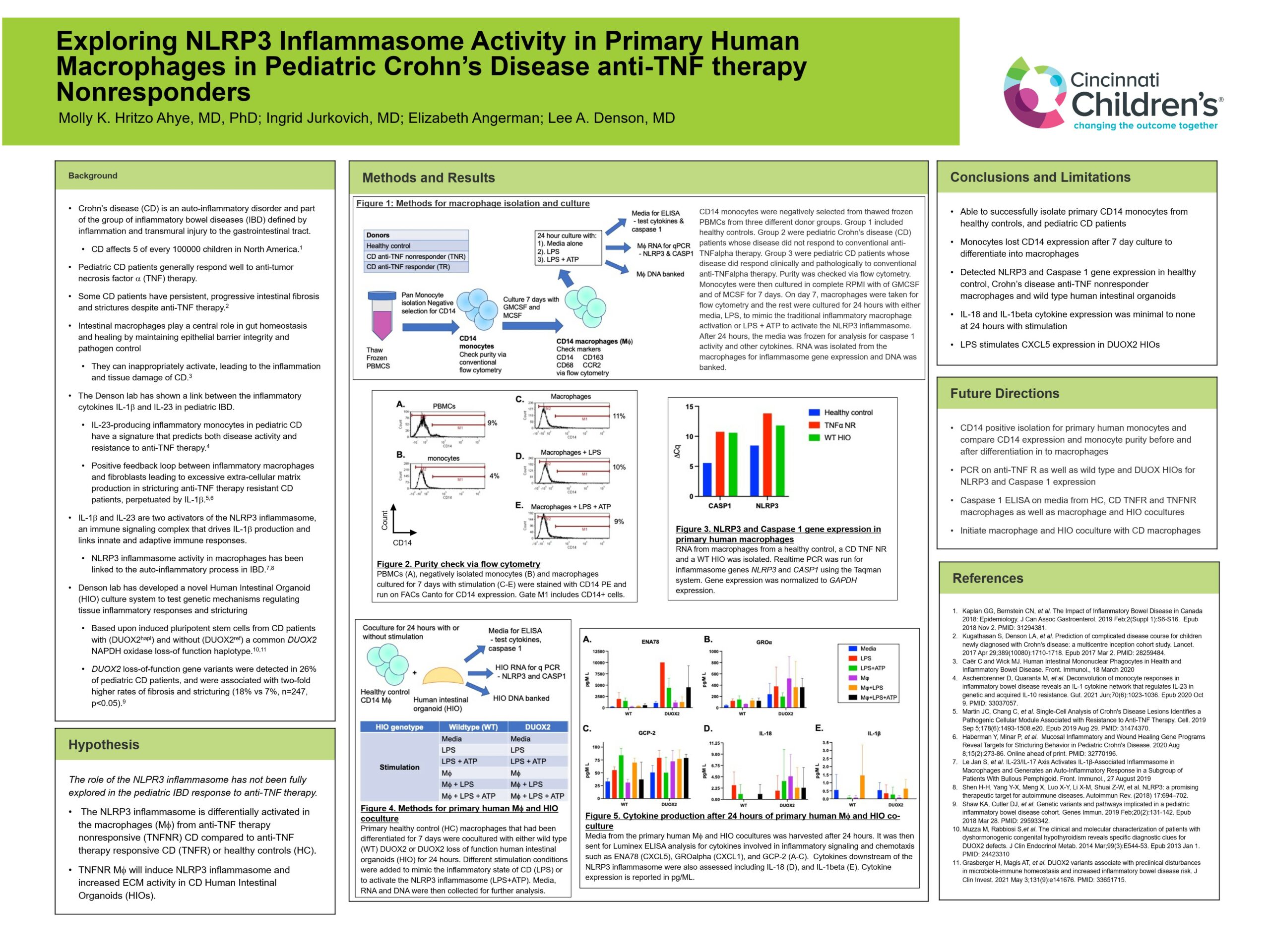
Background: Crohn’s disease (CD) is an auto-inflammatory disorder and part the inflammatory bowel disease group (IBD). Pediatric CD patients generally respond well to anti-tumor necrosis factor a (TNF) therapy. However, some CD patients have persistent intestinal fibrosis and strictures despite anti-TNF therapy. Intestinal macrophages play a critical part in epithelial barrier integrity and pathogen control by activating an appropriate immune response. However, they can also be inappropriately activated, leading to the inflammation and damage of CD. The Denson lab and collaborators have shown a link between the inflammatory cytokines IL-1b and IL-23 and pediatric IBD. Additionally, they demonstrated that there is a likely positive feedback loop between inflammatory macrophages and fibroblasts leading to excessive extra-cellular matrix production in stricturing anti-TNF therapy-resistant CD patients, perpetuated by IL-1b. IL-1b and IL-23 activate the NLRP3 inflammasome, an immune signaling complex that drives IL-1b production and links innate and adaptive immune responses. NLRP3 inflammasome activity in macrophages has been linked to the auto-inflammatory process in IBD.
Objective: However, the role of the NLPR3 inflammasome has not been fully explored in the pediatric IBD response to anti-TNF therapy. We tested the hypothesis that the NLRP3 inflammasome is differentially activated in the macrophages from anti-TNF therapy nonresponsive (TNFNR) CD compared to anti-TNF therapy responsive CD (TNFR) or healthy controls (HC).
Methods: CD14 positive primary human monocytes were isolated from HC and CD patients, either TNFR or TNFNR. Macrophages were induced and then activated with either LPS, to mimic the inflammatory state of CD, or LPS and ATP to activate the NLRP3 inflammasome. RNA was isolated and RT-PCR was used to quantify CASP1 and NLRP3 gene activity.
Results: LPS and ATP did activate both CASP1 and NLRP3 in HC macrophages, but CD samples had nonquantifiable amount of RNA.
Conclusions: We have redemonstrated that LPS and ATP induce NLRP3 inflammasome gene activity in primary human HC macrophages. We will repeat cultures to quantify inflammasome gene activity in TNFR and TNFNR CD macrophages. We will also coculture macrophages with a novel CD-derived human intestinal organoid system developed in the Denson lab to explore the effects of macrophages on inflammasome activity in CD intestinal cells.