Feasibility and Comparison of Early-Onset Sepsis Risk-Stratification Calculators in Late Preterm and Term Neonates in a Kenyan Nursery
Lindsey Fileccia, MD; Alyssa Guthrie, BS; Tristan Wood, BS; Joshua Schaffzin, MD, PhD, MPH, FAAP; Chunyan Liu, MS; Cynthia Ronoh, KRN; Beena Kamath-Rayne, MD, MPH, FAAP; Amy Rule, MD, MPH, FAAP
Risk Stratification Algorithms for Early Onset Sepsis can feasibly be implemented in Low and Middle Income Country nurseries and have the potential to decrease duration of antibiotic administration and length of stay.
-Lindsey Fileccia, MD
Abstract
Background: Risk stratification algorithms (RSAs) can reduce antibiotic use and hospitalization in neonates >35wks at risk for Early Onset Sepsis (EOS) in high-income nations. Low- and middle-income countries (LMIC) experience greater EOS burden, increasing antibiotic resistance rates, and have limited capacity for laboratory studies.
Objective: 1) To evaluate the feasibility of applying EOS RSAs in a LMIC nursery. 2) To compare the impact of four existing RSAs on antibiotic duration (AD) and length of stay (LOS) in a LMIC nursery.
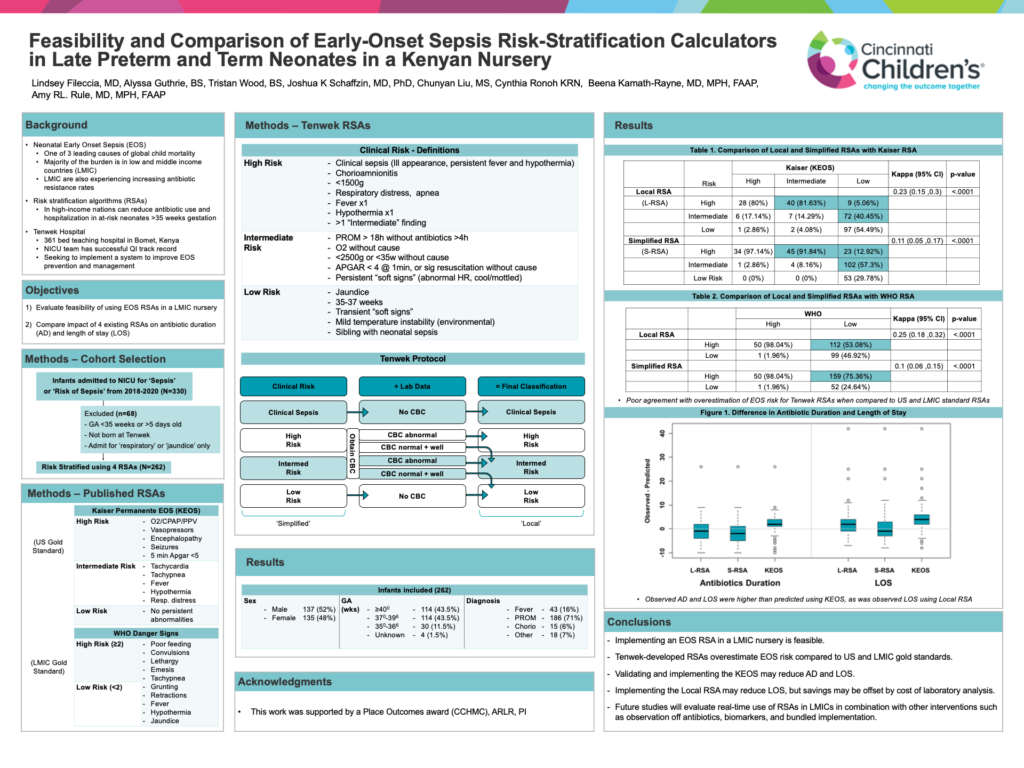
Methods: We included 262 neonates admitted at <5d for presumed sepsis at Tenwek Hospital (Bomet, Kenya) during 2018-2020 who were >35wk. RSAs used included the current local sepsis protocol (‘local RSA’, combines maternal and neonatal clinical and laboratory data), a simplified local protocol (‘simplified RSA’, excludes laboratory data), the Kaiser-Permanente EOS clinical assessment (‘KEOS’, US gold standard), and the World Health Organization Danger Signs (LMIC gold standard). Each patient was classified as high, moderate, or low risk of EOS for each RSA. We evaluated agreements between RSAs using Kappa coefficients and direction of disagreement with McNemar’s test. Differences in observed and predicted median AD and LOS were evaluated using the Wilcoxon signed rank test.
Results: 229 (87%) neonates were term, 34 neonates were 35-36wks. 137 (52%) were male. Both the local and simplified RSAs agreed poorly with both gold standard RSAs. The simplified RSA overestimated EOS risk compared to the local RSA; both local and simplified RSAs overestimated risk compared to the standard RSAs. AD was shortened by two days using the KEOS, and lengthened by two days using the simplified RSA. LOS was shortened by four days using the KEOS and by two days using the local RSA.
Conclusions: The local RSA overestimated EOS risk compared to the gold standard. However, if implemented fully, both the local RSA and the KEOS may reduce AD and LOS. Further study is needed to determine if savings from LOS are offset by the cost of laboratory testing. Future studies will evaluate the real-time use of RSAs in LMICs in combination with other interventions such as observation off antibiotics, biomarkers, and bundled implementation.