Impact of Fit Kits for Fit Kids Intervention on Primary Care Pediatric Weight Management
Katelyn Gordon MD, Aeesha Ranavaya MD, Jais Emmanuel MD, Richard Droghini MD, Sarah Reel MD, Ghazal Rashidi MD, Leonardo Ferreira MD, Madeline Weber MD, Mary Carol Burkhardt MD MHA, Robert Siegel MD FAAP
The Fit Kits for Fit Kids Intervention demonstrated a positive impact on patients, families, and providers in the setting of primary care pediatric weight management.
Katelyn Gordon, MD & Aeesha Ranavaya, MD
Abstract
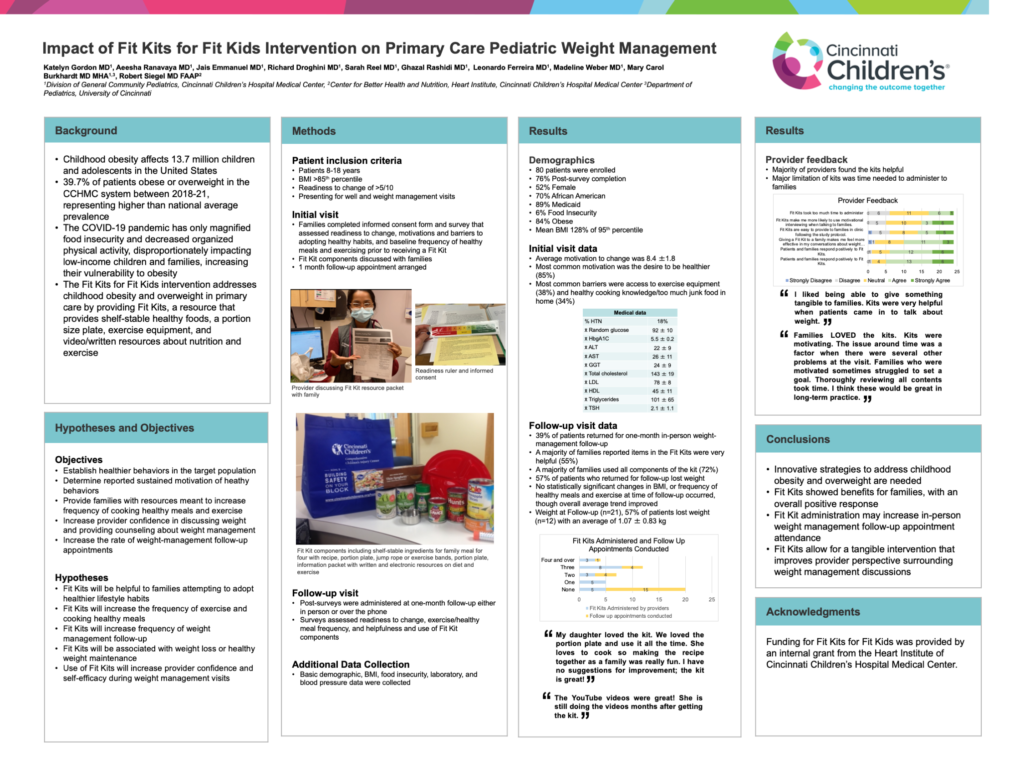
Background: Childhood obesity affects 13.7 million children and adolescents in the United States, with 39.7% of patients obese or overweight in the CCHMC system between 2018-21, representing a higher than national average prevalence. The COVID-19 pandemic magnified food insecurity and decreased organized physical activity, disproportionately impacting low-income families, increasing their vulnerability to obesity. The Fit Kits for Fit Kids intervention addresses childhood obesity and overweight in primary care by providing Fit Kits, a resource that provides shelf-stable healthy foods, a portion size plate, exercise equipment, and video/written resources about nutrition and exercise.
Objective: To establish healthier behaviors in the target population, and to determine reported sustained motivation of heathy behaviors, use of Fit Kit contents, increased frequency of cooking healthy meals and exercise, and the rate of weight-management follow-up appointments for patients who received Fit Kits.
Methods: Patients 8-18 years, with BMI >85th percentile and readiness to change of >5/10 presenting for well visits were recruited, and completed a survey that assessed readiness to change, motivations and barriers to adopting healthy habits, and baseline frequency of healthy meals and exercising prior to receiving a Fit Kit. Post-surveys were administered at one-month follow-up, and assessed readiness to change, exercise/healthy meal frequency, and helpfulness and use of Fit Kit components. Basic demographic, BMI, food insecurity, laboratory, and blood pressure data were collected.
Results: At time of analysis, 80 patients were enrolled, with 76% post-survey completion; 52% female, 70% African American, 84% obese, mean BMI 128% of 95th percentile. 39% of patients returned for one-month in-person weight-management follow-up. The most common motivation was the desire to be healthier (85%) and most common barriers were access to exercise equipment (38%) and healthy cooking knowledge/too much junk food in home (34%). A majority of families reported items in the Fit Kits were very helpful (55%) and used all components of the kit (72%). No statistically significant changes in BMI, or frequency of healthy meals and exercise at time of follow-up occurred, though overall average trend improved.
Conclusions: Innovative strategies to address childhood obesity and overweight are needed. Fit Kits showed benefits for families, with an overall positive response, and administration may increase in-person weight management follow-up appointment attendance.