Factors Associated with Acute Kidney Injury During Treatment of CNS Malignancies
Heepke Knickel, MD; Ralph Salloum, MD; Elizabeth Rompies, MSN, APRN, CNP;
Kelli Krallman, RN, BSN, MS, CCRC; Stuart Goldstein, MD, FAAP, FNKF
Receiving CSI or chemotherapy is associated with AKI development during treatment of CNS malignancies.
-Heepke Knickel, MD
Abstract
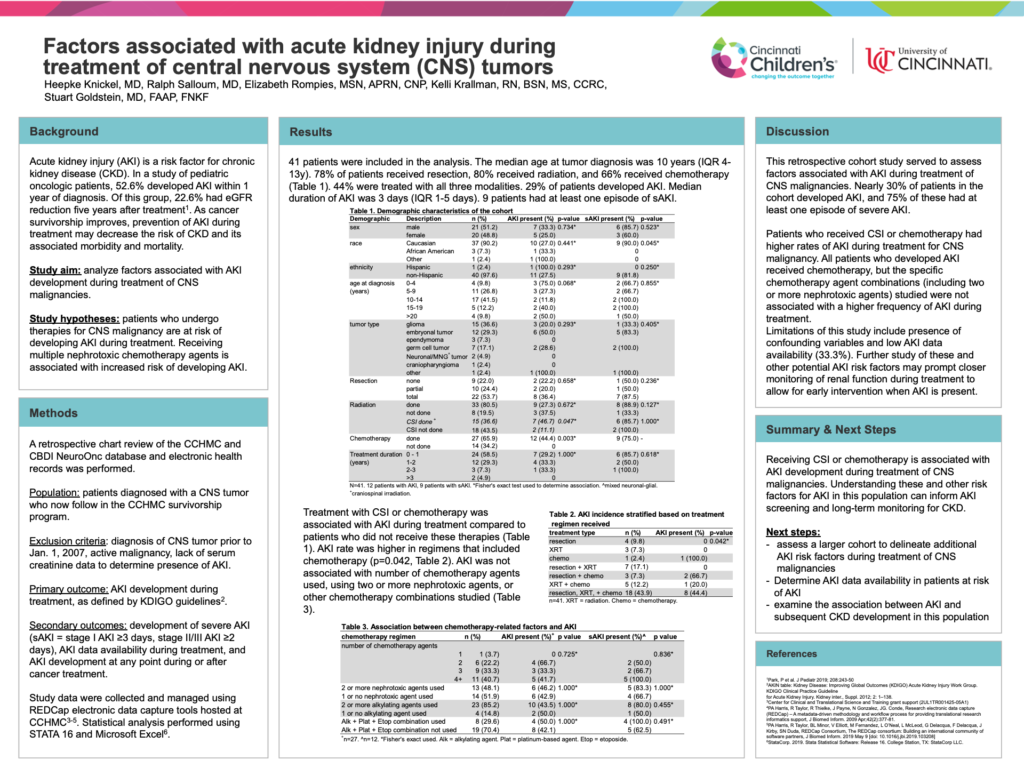
Background: Acute kidney injury (AKI) is a risk factor for chronic kidney disease (CKD). In a study of pediatric oncologic patients, 52.6% developed AKI within 1 year of diagnosis. Of this group, 22.6% had eGFR reduction five years after treatment1. As cancer survivorship improves, prevention of AKI during treatment may decrease the risk of CKD and its associated morbidity and mortality. Few studies have assessed the risk of AKI in children treated for central nervous system (CNS) tumors. This study sought to analyze factors associated with development of AKI during treatment of these malignancies.
Hypothesis: Patients who undergo therapies for CNS malignancy are at risk of developing AKI during treatment. Receiving multiple nephrotoxic agents is associated with increased risk of developing AKI.
Methods: Charts of patients diagnosed with a CNS malignancy between January 2007 and July 2015 and following in the CCHMC survivorship program were reviewed. Data for demographic and therapy-related factors were collected. The primary outcome was AKI development during treatment, as defined by KDIGO guidelines. Secondary outcomes included development of severe AKI and AKI data availability during treatment.
Results: 43 patients were available for analysis. The most common tumor types were glioma, embryonal tumor, and germ cell tumor. 33 patients underwent resection, 35 received radiation, and 27 received at least one chemotherapy agent. 18 patients received all three therapies. AKI was noted in 16 patients, 11 of whom had at least one severe AKI episode. Factors associated with AKI included tumor type (p=0.03), craniospinal radiation (p=0.002), and use of two or more nephrotoxic chemotherapy agents (p=0.006).
Conclusions: Tumor type, nephrotoxic chemotherapy, and craniospinal radiation are associated with AKI during CNS cancer therapy. Presence of these factors may prompt closer monitoring of renal function during treatment and early intervention when AKI is present. Limitations of this study include sample size, confounding variables, and AKI data availability. Next steps involve assessing a larger cohort to delineate additional AKI risk factors and examining the association between AKI and subsequent CKD development in this population.