Improving Immunization Rates in Underserved Neighborhoods
Erin McCann, MD, MPH; Deawodi Ladzekpo, MD; Elizabeth Lendrum, MD;
Mary Carol Burkhardt, MD, MHA; Melissa Klein, MD, MEd
Vaccine educational materials that address family concerns and learning preferences may enhance quality of conversations and ultimately decrease immunization refusal in our community.
-Erin McCann, MD, MPH, Deawodi Ladzekpo, MD, & Elizabeth Lendrum, MD
Abstract
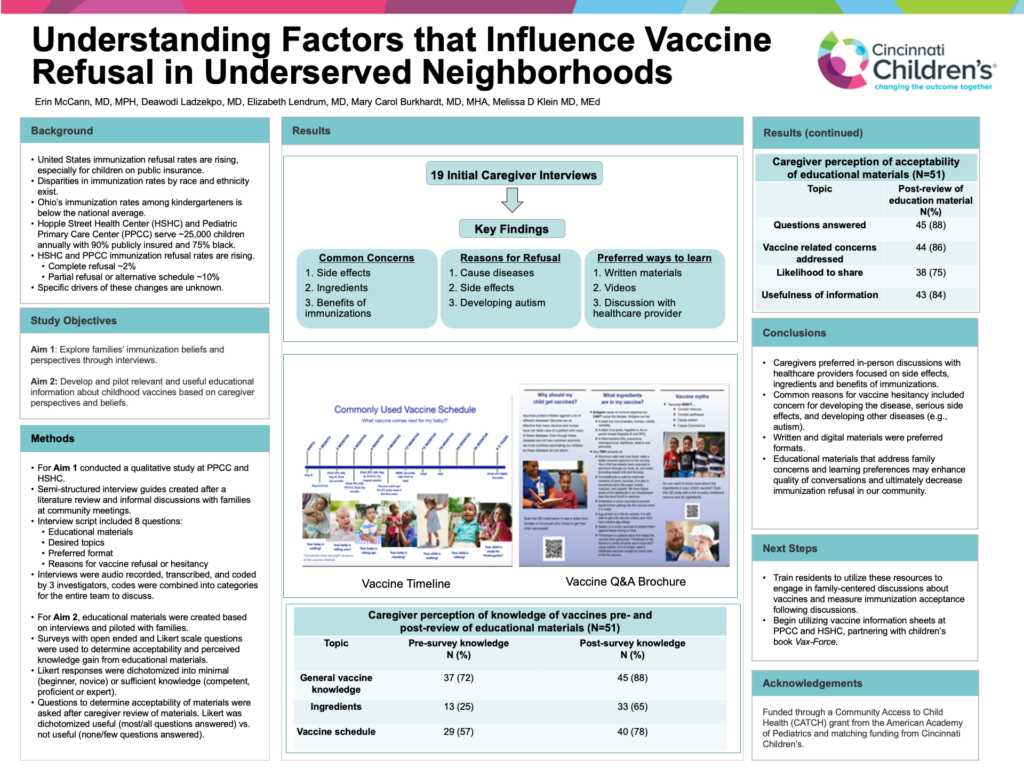
Background: Immunization refusal rates in the United States are increasing. Ohio is below the national average for immunization rates, with even lower rates among children who are publicly insured. Our two hospital-based continuity clinics serve 25,000 children from urban, underserved neighborhoods, with 90% publicly insured and 75% Black. Our immunization refusal rate is 2%, but nearly 10% of families refuse select immunizations or request alternative schedules. The drivers of decreasing local immunization rates are unknown.
Objective: To explore families’ immunization beliefs and perspectives through interviews.
Methods: This qualitative study took place at a large, urban children’s hospital. Caregivers of patients at two hospital-affiliated clinic sites were recruited. We developed semi-structured interview guides after conducting a literature review and holding informal discussions with families at community meetings. The interview script included eight questions related to educational materials, desired topics, preferred format and reasons for vaccine refusal. Interviews were audio recorded, transcribed and coded by one team member, then collectively analyzed by three team members to identify commonalities. Educational materials were created based on interviews and piloted with families to determine acceptability and seek feedback.
Results: Eighteen interviews were conducted. Key educational topics identified included vaccine ingredients, side effects, and general benefits of immunizations. Reasons for vaccine refusal included concerns that vaccines cause disease, side effects, and a fear of developing autism. Written materials and videos were the preferred educational format, and families wanted these materials to accompany in-person discussions with their providers.
Conclusion: Caregivers indicated preferences for written and digital materials to augment vaccine- related discussions with healthcare providers. Developing educational materials that address family concerns and learning preferences may enhance quality of conversations and ultimately decrease immunization refusal in our community. Next steps include finalizing educational materials and training residents to utilize these resources to engage in family-centered discussions.