Potentially Avoidable Transfers to the Pediatric ICU
Ellen Pittman, MD; Tina Sosa, MD; Patrick Brady, MD, MSc; Ken Tegtmeyer, MD; Maya Dewan, MD, MPH
We have successfully decreased the number of pediatric cardiac arrests that occur outside the ICU. However, this means some patients are transferred to the ICU that may have been safe to remain on the floor. If we can understand the key drivers of these transfers, we can design quality improvement initiatives to reduce potentially avoidable transfers to the pediatric ICU.
-Ellen Pittman, MD
Abstract
Background: To reduce pediatric in-hospital cardiac arrests, many institutions have implemented rapid response teams to identify patients at risk for deterioration and intervene prior to their decompensation. To avoid deterioration in general care areas, some patients are transferred to the ICU who do not require ICU level interventions. These patients may have remained safely on the floor, but with less healthcare utilization and potentially lower healthcare costs. However, there is little known about this subset of patients and more understanding is needed to help improve value while preserving patient safety.
Objective: To describe the cohort of patients who are transferred from a general floor to the PICU and who cannot be classified as a critical deterioration event (CDE) or emergency transfer (ET).
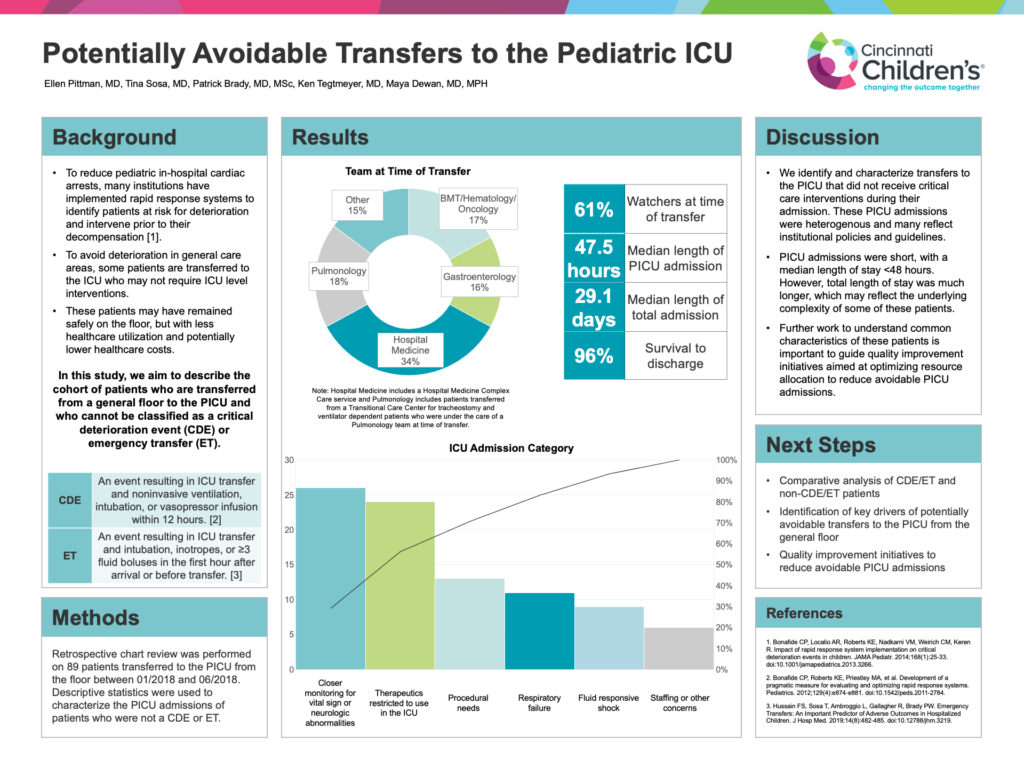
Methods: Retrospective chart review was performed on 89 patients transferred to the PICU from the floor from January 2018 – June 2018. Patients who did not meet criteria for CDE or ET were identified, and descriptive statistics were used to characterize these PICU admissions.
Results: Of the 89 patients, 34% were transferred from Hospital Medicine, including a Hospital Medicine Complex Care service, 18% from Pulmonary in a Transitional Care Center for tracheostomy and ventilator dependent patients, 17% from Hematology/Oncology/BMT, and 16% from Gastroenterology. Sixty-one percent were “watchers”, or patients labeled at risk for deterioration, on the floor prior to transfer. The types of ICU admissions for these patients were heterogenous, including acute on chronic respiratory failure (9%), transfer for procedural needs (15%), the need for treatments whose use is restricted to the ICU (22%), and closer monitoring in the setting of vital sign instability (16%). Median length of PICU admission was 47.5 hours. Median length of total admission was 29.1 days, and 96% of patients survived to discharge.
Conclusions: In this interim analysis we identify and characterize a cohort of patients transferred to the ICU that did not go on to receive critical care interventions during their PICU admission. Further work to understand common characteristics of these patients is important to guide quality improvement initiatives aimed at optimizing resource allocation to reduce avoidable PICU admissions.