Identifying Health-Harming Social Needs among Patients Presenting to a Pediatric Urgent Care
Elizabeth C. Lendrum, MD; Kristen Peterson, MD; Mike A. Gittelman, MD; Melissa D. Klein, MD, MEd; Wendy J. Pomerantz, MD, MS; Andrew F. Beck, MD, MPH
Half of guardians of young patients visiting an urgent care experience at least one health-harming social need. Routine screening of social needs in urgent care is warranted.
Elizabeth Lendrum, MD
Abstract
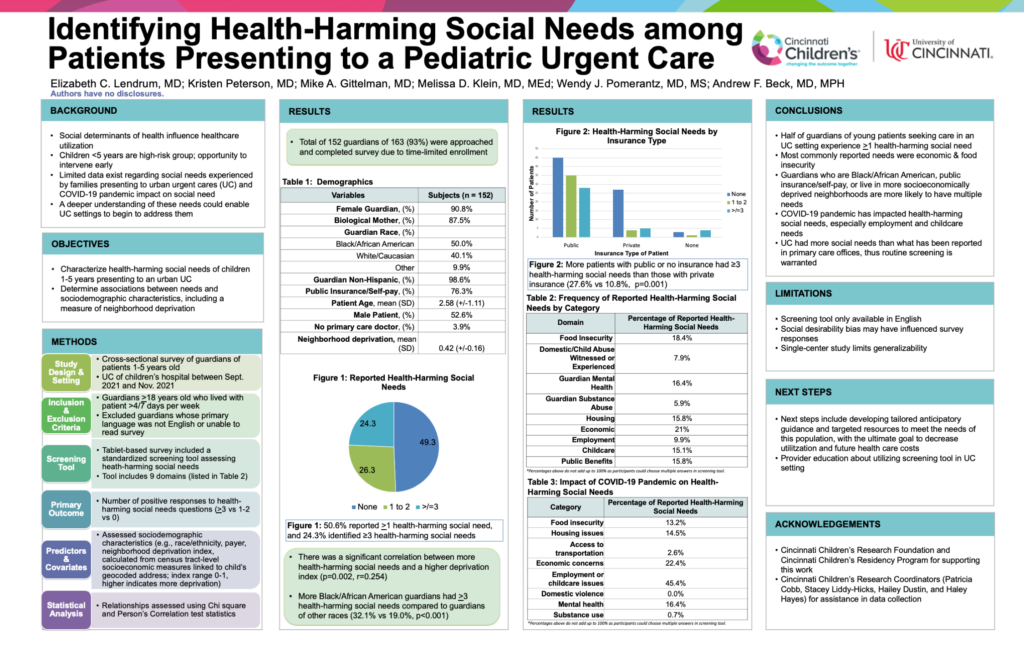
Background: Social determinants of health influence healthcare utilization. Limited data exist regarding social needs experienced by families presenting to an urban urgent care (UC). A deeper understanding of these needs could enable UC settings to begin to address them.
Objective: To characterize health-harming social needs (HHSN) of children 1-5 years old presenting to a pediatric UC and to determine the association between these needs and patient sociodemographic characteristics.
Methods: This was a cross-sectional study that surveyed guardians of patients aged 1-5 years who presented to the UC of a children’s hospital between 9/21 and 11/21. The survey, completed via tablet, included a standardized screening tool assessing HHSN. Guardians ≥18 years who lived with the patient >4/7 days per week were included; those whose primary language was not English or who were unable to read the survey were excluded. We tabulated the number of reported HHSN (e.g., food insecurity). Our primary outcome was the number of positive responses to HHSN questions (≥3 vs 1-2 vs 0). Assessed sociodemographic characteristics included race/ethnicity, patient age, insurance status, and neighborhood deprivation index, calculated from census tract-level socioeconomic measures linked to the child’s geocoded address (index range 0-1, higher indicates more deprivation). We assessed relationships using Chi square, ANOVA, and Pearson’s Correlation test statistics.
Results: A total of 152 guardians (50.0% non-Hispanic Black, 90.8% female, 87.5% biological mother) completed the survey. More than half (50.6%) reported ≥1 HHSN, and 24.3% identified ≥3. HHSN category was not associated with patient age, race/ethnicity, or guardian age. More Black guardians had ≥3 HHSN than guardians of other races (32.1% vs 19.0%, p<0.001); more patients with public or no insurance had ≥3 HHSN than those with private insurance (27.6% vs 10.8%, p=0.001). Economic concerns and food insecurity were the most common HHSNs identified. There was a significant correlation between more HHSN and a higher deprivation index (p=0.002, r=0.254).
Conclusions: Many guardians of young patients seeking care in an UC experience at least one HHSN. Those who are Black with public or no insurance were more likely to have multiple risks. Identifying HHSN through screening may allow for providing resources in an UC setting.
Table 1: Health-Harming Social Needs
| Number of Reported HHSN | % (n=152) |
| 0 | 49.3% |
| 1-2 | 26.3% |
| ≥3 | 24.3% |
| Frequency of Reported HHSN by Category | % (n)* |
| Food Insecurity | 18.4% (28) |
| Domestic/Child Abuse Witnessed or Experienced | 7.9% (12) |
| Guardian Mental Health | 16.4% (25) |
| Guardian Substance Abuse | 5.9% (9) |
| Housing | 15.8% (24) |
| Economic | 21% (32) |
| Employment | 9.9% (15) |
| Childcare | 15.1% (23) |
| Public Benefits | 15.8% (24) |
*Percentages above do not add up to 100% as participants could choose multiple answers in screening tool.