Cardiac Histopathology in Duchenne Muscular Dystrophy: Novel Findings and Implications for Therapy
Eleanor Greiner, MD; Jennifer Kasten, MD, MSc; Samuel Wittekind, MD; Thomas D. Ryan, MD, PhD; Sean Lang, MD; Chet R. Villa, MD
Dilated Cardiomyopathy in Duchenne Muscular Dystrophy is characterized by diffuse fibrofatty replacement of the myocardium and conduction system which may contribute to conduction system disease and arrhythmias.
-Ellie Greiner, MD
Abstract
Background: Duchenne Muscular Dystrophy (DMD) is an X-linked disorder caused by mutations in the dystrophin gene. Loss of dystrophin leads to skeletal muscle weakness, respiratory failure, and cardiac dysfunction. Improvements in respiratory care and use of systemic corticosteroids have increased long term survival, leading to an increased burden of cardiac disease.
Objective: We sought to characterize the histopathologic findings in the myocardium of DMD patients and compare this to non-invasive cardiac diagnostic testing. We hypothesized that cardiac disease would be more extensive than the left ventricular fibrosis and dysfunction described by cardiac imaging.
Methods: Cardiac pathology samples obtained at left ventricular assist device (LVAD) placement or autopsy were reviewed for patients at CCHMC between 2010 and 2020. Autopsy specimens were generally limited to left ventricular tissue. A single patient had tissue specimens available for evaluation of all cardiac chambers and the conduction system. Serial cardiac imaging and EKGs were reviewed in conjunction with pathology samples.
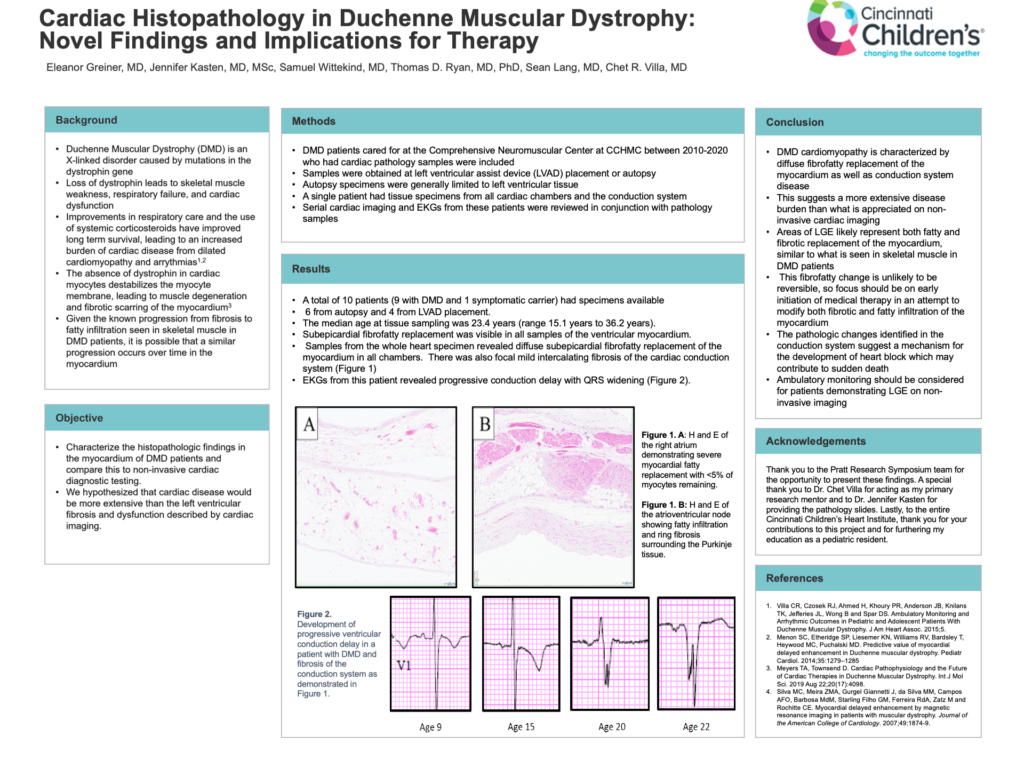
Results: A total of 10 patients (9 with DMD and 1 symptomatic carrier) had specimens available, 6 from autopsy and 4 from LVAD. The median age at tissue sampling was 23.4 years (range 15.1 to 36.2). Subepicardial fibrofatty replacement was visible to varying degrees in all samples of the ventricular myocardium. Samples from the whole heart specimen revealed diffuse subepicardial fibrofatty replacement of the myocardium in all chambers. There was also focal mild intercalating fibrosis of the cardiac conduction system (Figure 1). EKGs from this patient revealed progressive conduction delay with QRS widening (Figure 2).
Conclusions: This study demonstrates that DMD cardiomyopathy is characterized by diffuse, fibrofatty replacement of the myocardium as well as conduction system disease. Fibrofatty change is unlikely to be reversible and thus focus should be on early initiation of medical therapy in an attempt to modify disease progression. Furthermore, the pathologic changes identified in the conduction system suggest a mechanism for the development of heart block which may contribute to sudden death and warrants consideration of ambulatory monitoring.