Pneumatosis Intestinalis in Pediatric Liver and Small Bowel Transplant Recipients
Brianne Shuler, MD; Kathleen Campbell, MD
Pneumatosis intestinalis in post-solid organ transplant patients may have less morbidity and mortality than previously believed but further studies are needed to standardize management.
-Bri Shuler, MD
Abstract
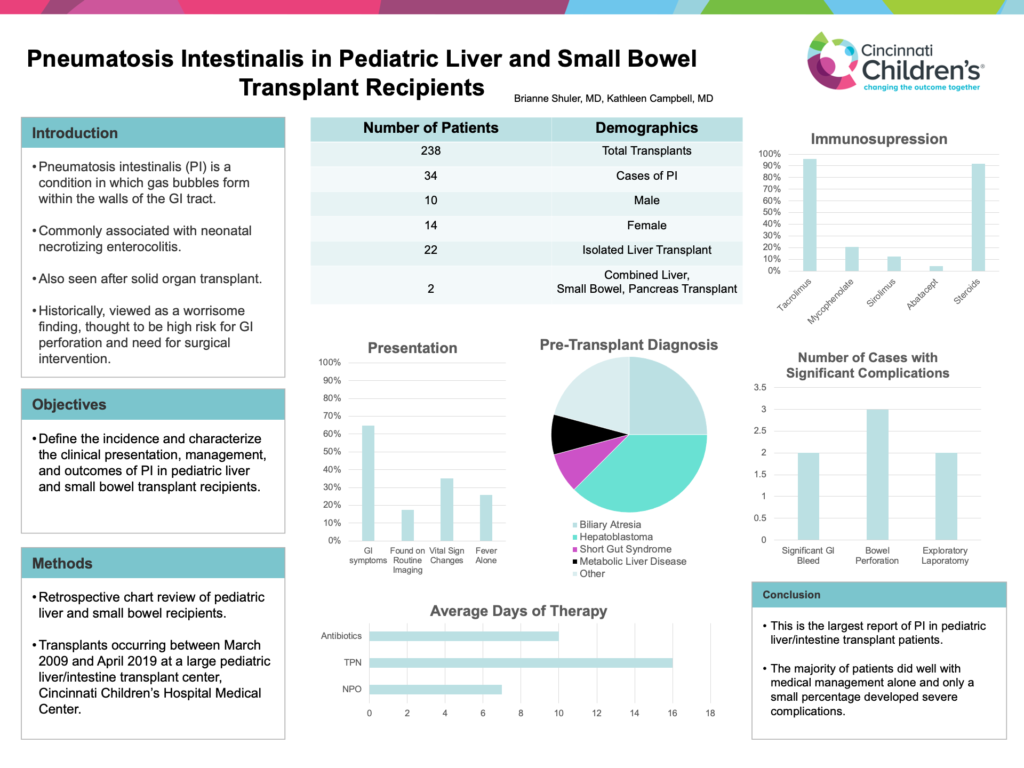
Background: Pneumatosis intestinalis (PI) is a condition in which gas bubbles form within the walls of the gastrointestinal tract. In pediatrics, this finding is commonly associated with necrotizing enterocolitis in the neonatal period but has also been described as a complication after solid organ transplant. Historically, PI has been viewed as a worrisome finding associated with high risk for gastrointestinal perforation and need for surgical intervention.
Objective: Our objective is to define the incidence and characterize the clinical presentation, management, and outcomes of PI in pediatric liver and small bowel transplant recipients.
Methods: This is a retrospective chart review of pediatric liver and small bowel recipients transplanted between March 2009 and April 2019 at a large pediatric liver/intestine transplant center.
Results: In this 10-year period, 238 transplants were performed in 230 patients. There were 34 cases of PI in 24 patients, representing 10% of all transplants and 10.4% of all patients. Cases included 10 males and 14 females, 92% isolated liver transplants and 8% combined liver, small bowel, pancreas transplants. Median time since transplant was 2.7 months. The initial diagnosis included 6 biliary atresia, 9 hepatoblastoma, 2 short gut syndrome, 2 metabolic liver disease, and 5 other. During the episodes of PI, 64.7% of cases presented with GI symptoms, 17.6% were found with routine imaging, 35% presented with vital sign changes and 26% with fever alone. 95.8% of patients were on Tacrolimus, 20.8% on Mycophenolate, 12.5% on Sirolimus, 4% on Abatacept, and 92% were on steroids at the time of diagnosis. All patients were made NPO and received IV antibiotics. Average days of NPO, TPN, and antibiotic therapy were 7, 16, and 10 respectively. 8 cases tested positive for enteric infections at the time of PI, and 5 patients developed bacteremia within 14 days of PI diagnosis. 2 patients had significant GI bleeds, 3 had bowel perforations, and 2 required exploratory laparotomy concurrent with development of PI.
Conclusions: This is the largest report of PI in pediatric liver/intestine transplant patients. The majority of patients did well with medical management alone and only a small percentage developed severe complications.