Retrospective Review of Premature Infant Respiratory Outcomes Following Late Postnatal Steroid Administration
James Rowe, MD; Jessica Kris, MD; Audrey Walters, BA; Melissa House, MD; Shawn Ahlfeld, MD
Infants requiring tracheostomy required more steroid courses, with courses greater than 3 days duration, were transferred later to a quaternary center, had treatment initiated later and required higher mean airway pressures at time of therapy and at therapy completion.
-Andy Rowe, MD & Jessica Kris, MD
Abstract
Background: Preterm infants with evolving or established bronchopulmonary dysplasia (BPD) are often administered systemic corticosteroids. Despite exposure to corticosteroids, many infants will ultimately require tracheostomy. Clinical characteristics of corticosteroid therapy in those that eventually require tracheostomy have not been well described but may be helpful to identify early on infants at highest risk.
Objective: To compare clinical characteristics (timing, number of courses, and response to corticosteroid administration) in premature infants that eventually liberated from PPV to those that ultimately required tracheostomy.
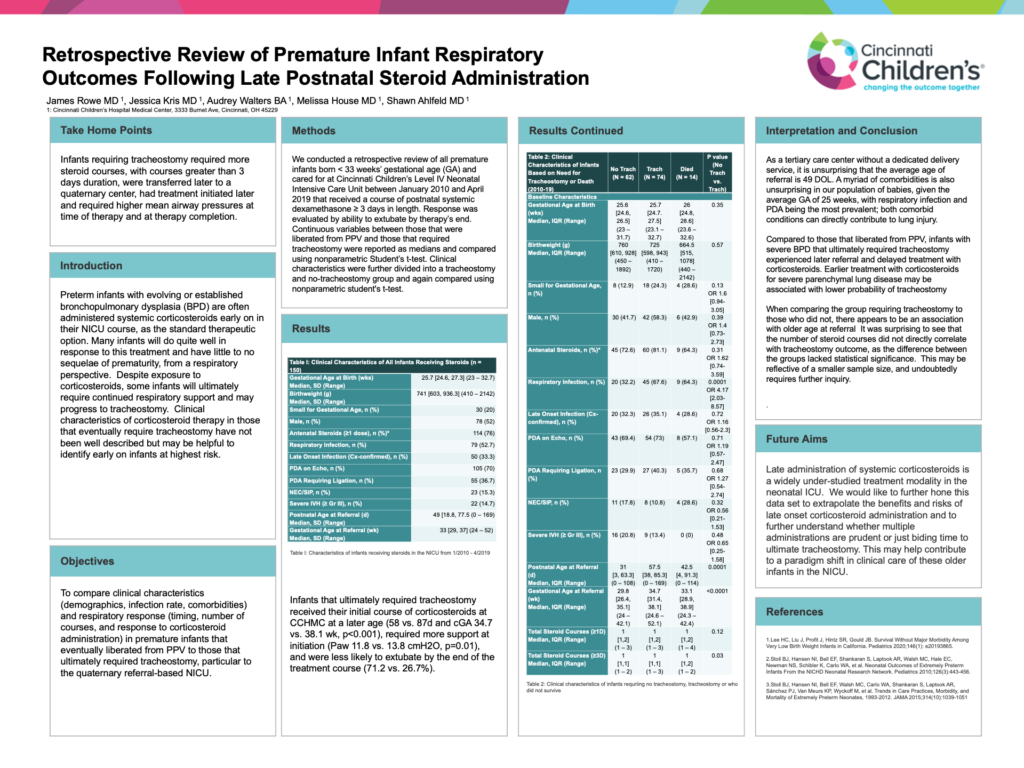
Methods: We conducted a retrospective review of all premature infants born < 33 weeks’ gestational age (GA) and cared for at Cincinnati Children’s Level IV Neonatal Intensive Care Unit between January 2010 and April 2019 that received a course of postnatal systemic dexamethasone ≥ 3 days in length. Response was evaluated by ability to extubate by therapy’s end. Continuous variables between those that were liberated from PPV and those that required tracheostomy were reported as medians and compared using nonparametric Student’s t-test.
Results: During the nine-year study period, 158 infants received a course of corticosteroids ≥3 days in length and 67 of those infants (42.4%) ultimately required tracheostomy at a median 128 days of age and 44.1wk corrected GA (cGA). The two groups had similar birth weights (BW) and birth GA (770g vs. 710g and 25.6 vs. 25.7wk, respectively). Infants that ultimately required tracheostomy were referred to CCHMC at a later postnatal age (38 vs. 57d and cGA 31.9wk vs. 34.7wk, p<0.01), received their initial course of corticosteroids at CCHMC at a later age (58 vs. 87d and cGA 34.7 vs. 38.1 wk, p<0.001), required more support at initiation (Paw 11.8 vs. 13.8 cmH2O, p=0.01), and were less likely to extubate by the end of the treatment course (71.2 vs. 26.7%).
Conclusions: Compared to those that liberated from PPV, infants with severe BPD that ultimately required tracheostomy experienced later referral and delayed treatment with corticosteroids. Earlier treatment with corticosteroids for severe parenchymal lung disease may be associated with lower probability of tracheostomy.