Increasing Use of the Right Ventricle to Pulmonary Artery Shunt for Stage 1 Palliation: A Report from the National Pediatric Cardiology Quality Improvement Collaborative
Scott Wirth, MD; Haleh Heydarian, MD; Elisa Marcuccio, MD; Brooke Tepe, RN; Laurel Stein, RN; Garick Hill, MD
Surgical practice nationwide for the first stage repair of single ventricle heart disease appears to be changing in response to the information we have gleaned from the first and only randomized controlled trial comparing outcomes between two options for shunts in the Norwood Operation. Our study suggests this could be due to poorer outcomes associated with the modified Blalock-Taussig shunt.
-Hank Wirth, MD
Abstract
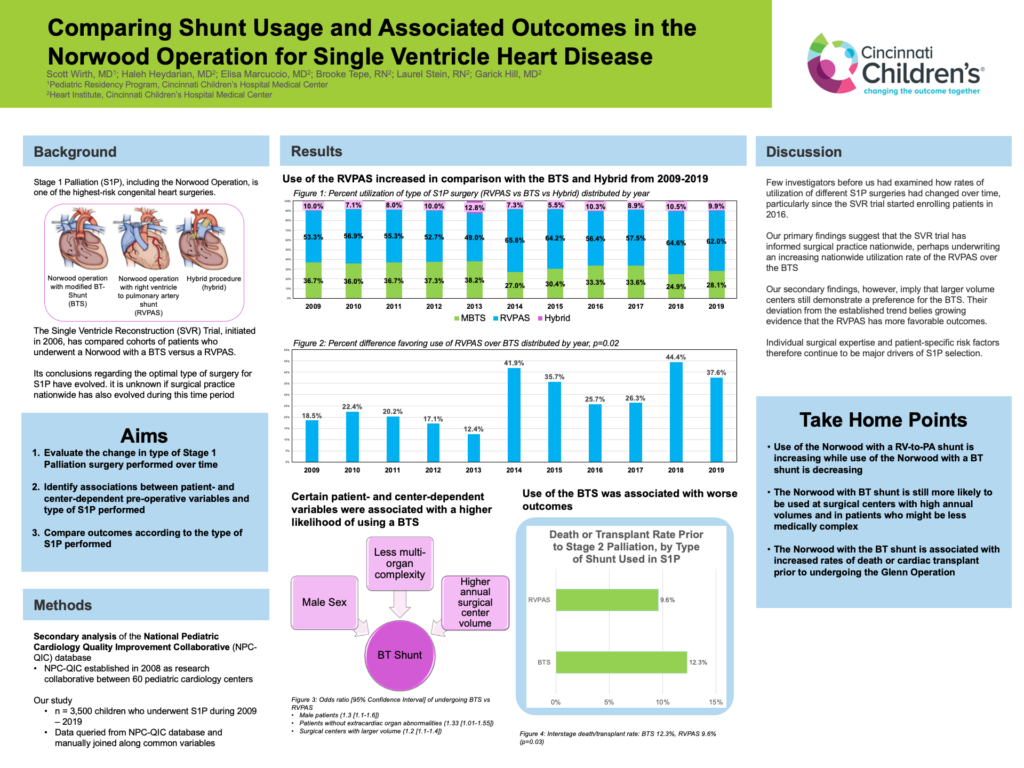
Background: Stage 1 palliation (S1P) of single ventricle heart defects with aortic hypoplasia consists of either the Norwood operation with a modified Blalock-Taussig shunt (MBTS) or a right ventricle-to-pulmonary artery shunt (RVPAS), or a hybrid procedure. Changes in national trends over time and factors influencing surgical approach remain unclear.
Objective: We aimed to assess changes in type of S1P utilized over time and associations between patient- and center-dependent risk factors and type of S1P performed. Additionally, we aimed to compare outcomes between types of S1P performed.
Methods: Data from the National Pediatric Cardiology Quality Improvement Collaborative (NPC- QIC) phase 1 (6/2008-8/2016) and phase 2 (8/2016-9/2019) databases were used. S1P type was evaluated by year of operation. Factors influencing the choice of MBTS versus RVPAS, as well as length of stay after S1P and death/transplant rates prior to Stage 2 palliation (S2P) between shunt types, were evaluated. Sites were stratified by the number of patients in the database per year as small (<5), medium (<10) and large (≥10) centers.
Results: The combined database included 3335 eligible patients; 1,028 (30.8%) with MBTS, 1,989 (59.7%) with RVPAS, and 318 (9.5%) with hybrid procedure. Overall, of 62 centers, 14.6% of S1P were at small centers (n=26), 40.6% at medium centers (n=24), and 44.7% at large centers (n=12). There was an increase in RVPAS use over time (p=0.02). In multivariable analysis, increasing hospital volume (OR 1.2 [95% CI 1.1-1.4], p=0.003) and absence of other organ system anomalies (OR 1.5 [95% CI 1.0-2.2], p=0.049) were associated with MBTS use over RVPAS. Median length of stay after S1P with MBTS was longer than with RVPAS (31 [95% CI 20-49] vs 29 [95% CI 19-47] days, p=0.054) and death/transplant rate was higher prior to S2P (12.3% vs 9.6%, p=0.03).
Conclusions: Use of RVPAS with S1P has increased over time with a decrease in MBTS use and unchanged hybrid frequency. MBTS is used more commonly in centers with higher volume and in patients without other anomalies but is associated with longer post-op hospitalization and lower transplant-free survival to stage 2 palliation.