Characteristics, Treatment, and Outcomes of Pediatric EBV Negative Monomorphic Post Solid Organ Transplant Lymphoproliferative Disorders [EBV(-)M-PTLD] – The Cincinnati Children’s Experience
Sarah McCormack, MD, Jeremy Rubinstein, MD, PhD
A retrospective study examining the characteristics, treatment and outcomes of pediatric EBV negative monomorphic post solid organ transplant lymphoproliferative disorders [EBV(-)M-PTLD] at Cincinnati Children’s Hospital Medical Center.
Sarah McCormack, MD
Abstract
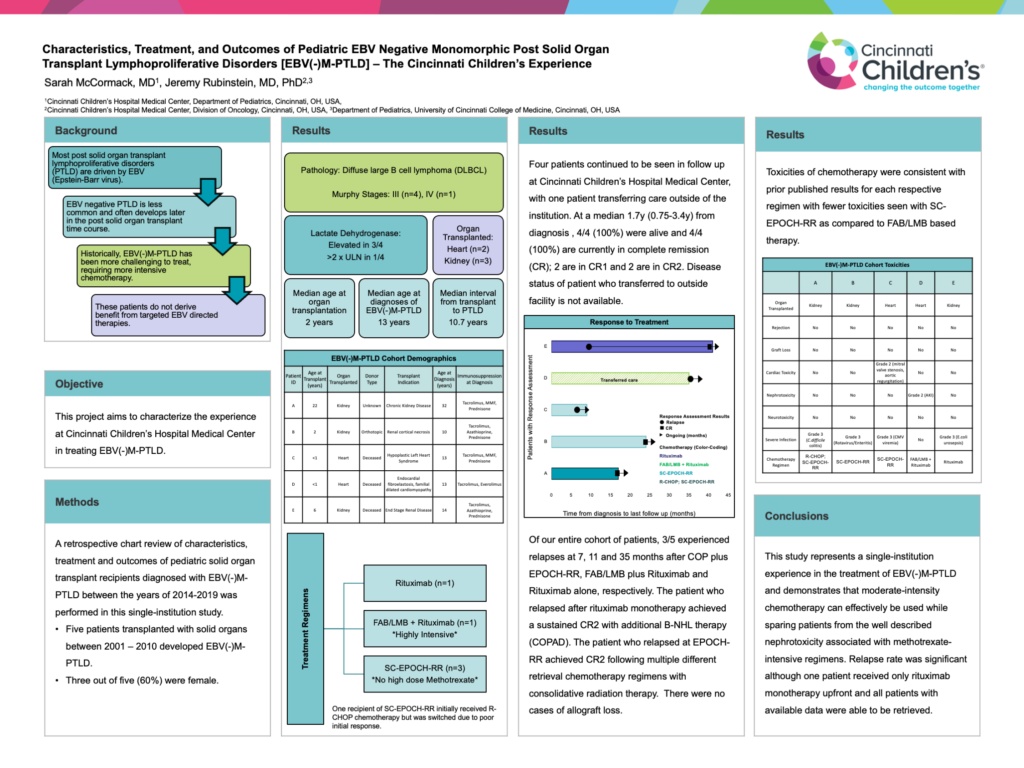
Background: Though the majority of post solid organ transplant lymphoproliferative disorders (PTLD) are driven by EBV (Epstein-Barr virus), there are an increasing number of cases of EBV negative PTLD that often develop later in the post solid organ transplant time course. EBV negative disease has historically been challenging to treat in pediatrics, requiring more intensive chemotherapy regimens. Additionally, patients do not derive benefit from the use of EBV-directed targeted therapies.
Objective: This project aims to characterize the experience at Cincinnati Children’s Hospital Medical Center in treating EBV(-)M-PTLD.
Methods: A retrospective chart review of characteristics, treatment and outcomes of pediatric solid organ transplant recipients diagnosed with EBV(-)M-PTLD between the years of 2014-2019 was performed in this single-institution study.
Results: Five patients transplanted with solid organs between 2001 – 2010 developed EBV(-)M-PTLD. Three out of five patients (60%) were female. Median age (range) at organ transplantation, diagnosis of EBV(-)M-PTLD and interval from transplant to PTLD were 2y (0.67-22), 13y (10-32) and 10.7y (8.2-13.8), respectively. Transplanted organs included heart (n=2) and kidney (n=3). Murphy stages were III (n=4) and IV (n=1). Lactate dehydrogenase was measured in 4/5 patients, was elevated in 3/4 (75%) and >2X upper limit of normal in 1/4 patients. All five patients were pathologically diagnosed with diffuse large B-cell lymphoma (DLBCL). Treatment included: Rituximab alone (n=1), highly intensive FAB/LMB plus Rituximab (n=1), moderately intensive SC-EPOCH-RR which lacks high-dose methotrexate (n=3). One recipient of SC-EPOCH-RR initially received R-CHOP chemotherapy but was switched due to poor initial response. Four patients continued to be seen in follow up at Cincinnati Children’s Hospital Medical Center, with one patient transferring care outside of the institution. At a median 1.7y (0.75-3.4y) from diagnosis , 4/4 (100%) were alive and 4/4 (100%) are currently in complete remission (CR); 2 are in CR1 and 2 are in CR2. Disease status of patient who transferred to outside facility is not available. Of our entire cohort of patients, 3/5 experienced relapses at 7, 11 and 35 months after COP plus EPOCH-RR, FAB/LMB plus Rituximab and Rituximab alone, respectively. The patient who relapsed after rituximab monotherapy achieved a sustained CR2 with additional B-NHL therapy (COPAD). The patient who relapsed at EPOCH-RR achieved CR2 following multiple different retrieval chemotherapy regimens with consolidative radiation therapy. There were no cases of allograft loss. Toxicities of chemotherapy were consistent with prior published results for each respective regimen with fewer toxicities seen with SC-EPOCH-RR as compared to FAB/LMB based therapy.
Conclusions: This study represents a single-institution experience in the treatment of EBV(-)M-PTLD and demonstrates that moderate-intensity chemotherapy can effectively be used while sparing patients from the well described nephrotoxicity associated with methotrexate-intensive regimens. Relapse rate was significant although one patient received only rituximab monotherapy upfront and all patients with available data were able to be retrieved.